Everything you need to know about the MMR vaccine…
And why you need to get it (even if you're an adult)
Last month, Aotearoa had its first confirmed case of measles since the first time since the 2019 outbreak.
That outbreak was the worst epidemic in New Zealand since an influenza epidemic in 1999, and is the worst measles epidemic since 1938. In Samoa, there were 83 deaths - 61 out of the first 70 deaths were little ones under four years old and all but seven were aged under 15. It was a devastating tragedy attributed decreased vaccination rates and someone from Aotearoa bringing measles into the country.
Here, two babies died in utero in the second trimester as a result of the outbreak.
Dr Ayesha Verrall has said she is “very concerned” about a possible measles outbreak, given the rates of vaccination in New Zealand. So I thought it was a good time to answer some questions about the MMR vaccine.
There has been a world-wide decline in vaccine rates and we’re saying that here - Ministry of Health data shows in the 12 months to December 31, 2022, only 67.5% of 18-month-olds had all age-appropriate childhood immunisations.
University of Auckland vaccinologist Dr Helen Petousis-Harris says this means an outbreak is inevitable. Public health Associate Professor Sir Collin Tukuitonga said as Māori and Pacific communities are known to be at risk of measles, they are likely to be “disproportionately affected”.
So, do your part, get vaccinated and talk to your loved ones about the MMR vaccine.
What is the MMR vaccine?
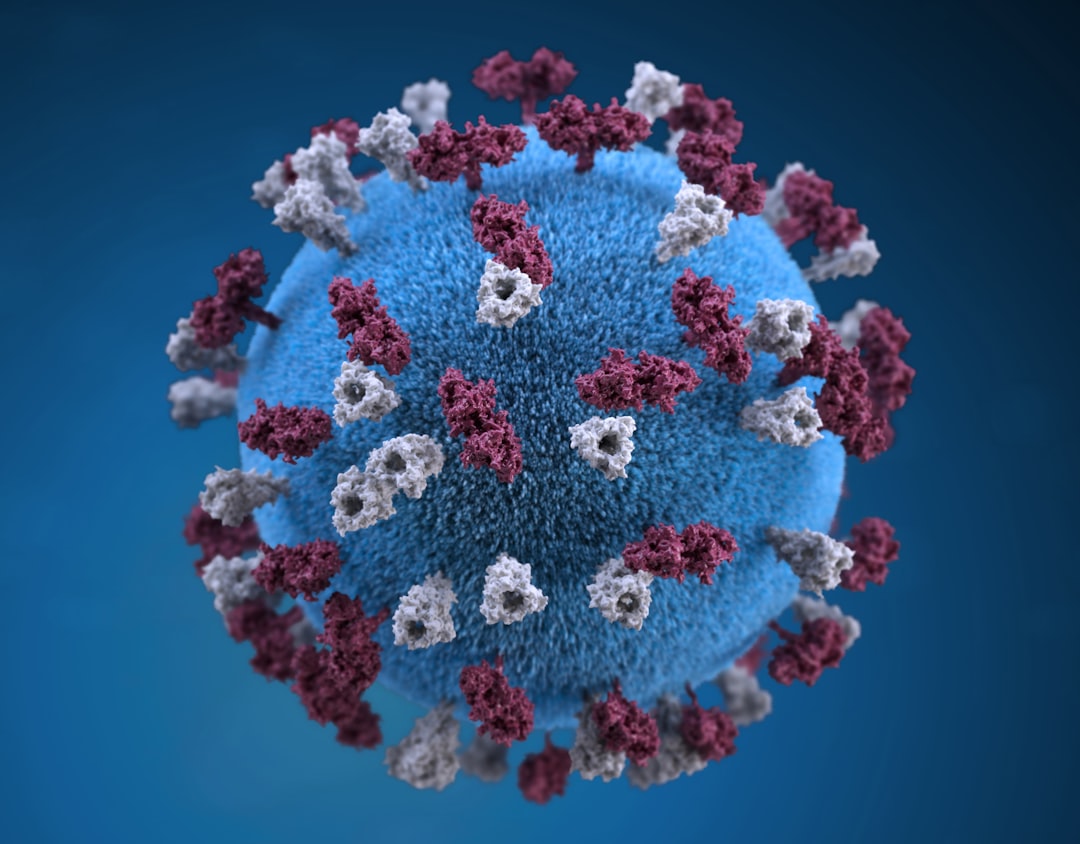
The MMR vaccine stands for Measles, Mumps and Rubella. The vaccine gives protection from these three viral infections.
The MMR vaccine is a live vaccine – this means that it is made using live viruses that have been weakened. After vaccination, the weakened vaccine teaches your body to recognise the viruses, so they can be quickly fought off if you ever catch the real things.
Who needs an MMR vaccine?
If you were born in or after 1969 and you haven’t already had two doses of the MMR vaccine, you should get it (and it’s free!).
Adults older than this were likely exposed to measles when they were younger, so don’t need the vaccine for measles. They may still need it for Mumps and Rubella though, so this is a good thing to chat to your doctor about it.
The MMR vaccine is one of the standard ones for children to get at 12 months and 15 months, so make sure they receive it too.
Why do we need it? And why should we vaccinate our kids?
The MMR vaccine is the best way to protect yourself from Measles, Mumps and Rubella. While these infections will only cause mild symptoms for some people, they can be serious for others. It is important for as many people as possible to have the MMR vaccine as it helps prevent those that are unable to have it (babies under the age of 12 months, pregnant women, people on some types of medication) from catching measles. It is also a great way for protecting your wider whānau.
The most important reason to vaccinate our kids is that they will be far less sick if they do catch one of these viruses in the future. Catching measles without being vaccinated gives you a 10% chance of ending up in hospital, and can cause diarrhoea, ear infections, pneumonia, and brain inflammation.
Death occurs in approximately 1 in 1,000 reported cases of measles, overall, in developed countries. Several years after infection, 1 in 100,000 measles cases will develop subacute sclerosing panencephalitis (SSPE), a degenerative brain disease; this condition is always fatal. Measles during pregnancy increases the risk of miscarriage and premature labour.
Mumps and rubella usually come with mild symptoms but sometimes they can be serious too – deafness and meningitis are risks for mumps, and rubella can be very dangerous for pregnant women.
You don’t want your kids having any of these! It’s far safer to get them vaccinated and protected.
Also as the mum of an immune compromised kid - I am deeply grateful to parents who get this vaccine. Lots of medically fragile kids can’t be vaccinated due to MMR being a live vaccine - we rely on our community to love our kids enough to get vaccinated to protect them. While measles can be a dangerous illness with long-term side effects for any child, it has a more than 50% death rate for New Zealand children with low immunity.
I think I was vaccinated as a kid but I don’t know and I can’t be bothered finding out, can I just be vaccinated again?
If you aren’t sure if you’ve had a vaccine or not, you’ve got a couple of options. You can either check your Well Child Tamariki Ora or Plunket book or ask your GP, or just go ahead and get a vaccine – there’s no safety worries about having extra doses.
Better to be safe than sorry by just getting vaccinated again.
How much does it cost to be vaccinated?
For most people, nothing! The MMR vaccine is free for everyone born in or after 1969 who hasn’t already had two recorded doses. You can get it at the same time as your flu or COVID-19 jab too, so you don’t even have to book in an extra trip to the doctor if you don’t want to.
I’m nervous about vaccines because my uncle says Donald Trump uses them to control our DNA…is the MMR vaccine safe?
Don’t listen to what your Uncle might be saying… there will be no DNA controlling and the vaccines don’t cause autism - in fact, those so called studies have been proven to be fabricated. They’re safe, tested, and approved by all sorts of doctors. It’s far more dangerous to cross the road than get a vaccine.
After the vaccine some folks have reported having a fever and/or mild rash for 6–12 days after immunisation for the measles component, fever and/or mild swelling under the jaw 10—14 days after immunisation for the mumps component and/or fever, mild rash and/or swollen glands two to four weeks after immunisation. Some people also report temporary joint pain two to four weeks after immunisation. This is more common in adult women than children. Much rarer responses are temporary low platelet count and convulsion associated with fever.
If you put this in perspective with the impact of measles on a strong immune system - people usually have an ear infection (acute otitis media), diarrhoea, pneumonia, low platelet count and a long-term weakened immune system.
What can I say to family about why they need to be vaccinated?
Encourage your whānau to get their vaccinations too if they haven’t had them. If it’s easier, head along at the same time for support, or start a conversation with them – some people may not realise how important the vaccine is.
If someone around you isn’t sure about getting a vaccine or whether it’s safe, that’s okay. Helping your family to understand the risks of not being vaccinated, and how much protection the vaccine can give them, can be a great first step.
What if I have a medically fragile child? Or a disabled child?
It is especially important that everyone around a vulnerable child - from their friends to their family, basically anyone who comes into contact with them - are immunised against measles. If they are not, they should keep away from them. If they have not been immunised, this should be done as soon as possible.
People can worry that they will give a vulnerable child measles from being vaccinated with the Measles, Mumps and Rubella vaccine because it is a live virus vaccine, but this is not a risk.
I want to send a huge thank you to Director of Nursing at healthcare provider ProCare, and Mum of two, Gabrielle Lord for helping me with the answers for this Q&A.



Even though I know I might get flamed by anti-vaxxers, measles could really hit our small town hard, so I've shared this to our local Facebook group. I know our medical centre has been trying to get the word out. Thanks for this information.
I sent out info about the whooping cough vaccine/booster to my workmates as we work in child health research and one realised she could get the MMR vaccinations too (US raised, unsure if she was vaccinated as a child) so she booked in straight away. I am so proud of my team!